
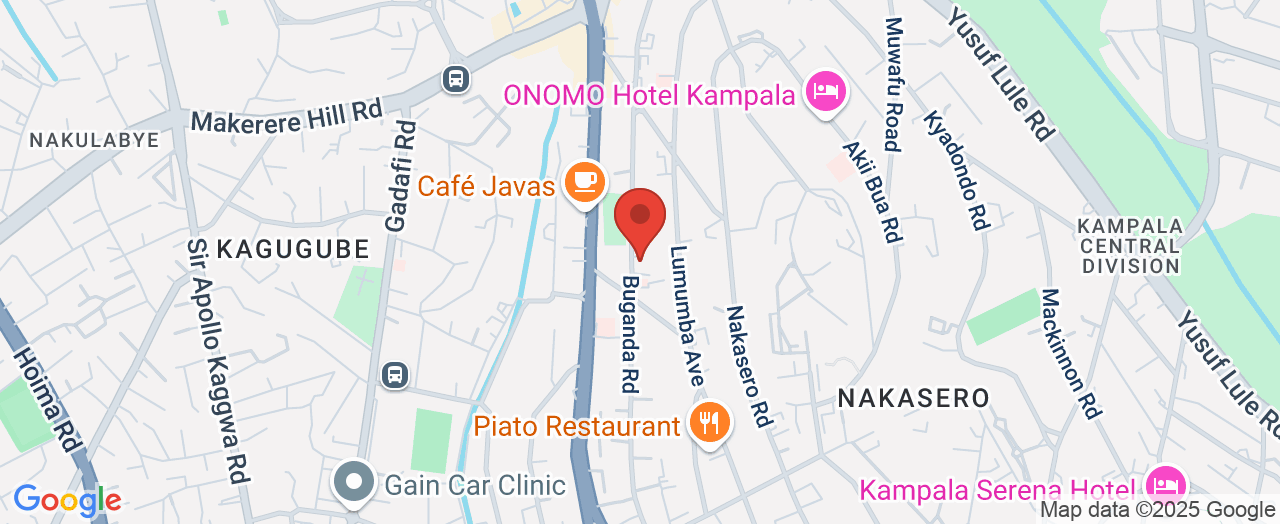
Case Medical Centre
📍 Address: 69 - 71 Buganda Rd,
📞 Phone: +256 800 211005
🌐 Website: https://casehospital.org/
★★★★★
Rating:3.7
Why Experience and Commitment Matter in Your Healthcare Journey
Imagine knowing that your health—and the health of your loved ones—rests in the hands of a medical institution with decades of unwavering dedication. In an ever-evolving world, where health threats can strike unexpectedly and access to critical care can feel daunting, the assurance of comprehensive, accessible medical expertise makes all the difference. The quest for holistic care—spanning from pediatric visits to emergency intervention—requires more than medical technology alone; it calls for a legacy of trust, adaptability, and integrated support that only time and consistent service can provide.
This is where the story of fluent healthcare unfolds, especially as families and individuals in Uganda navigate a landscape filled with healthcare choices and uncertainties. To become “fluent in healthcare” means having access to coordinated services, knowledgeable professionals, and infrastructure that can handle both everyday needs and sudden emergencies. Uganda’s dynamic healthcare setting, marked by both progress and challenge, places a premium on hospitals and insurance services that combine capacity, quality, and compassion. For over 25 years, some have refined this approach—supporting entire communities through preventive health, specialty medicine, and innovative insurance models. The consequences of not understanding or accessing such resources could mean delayed treatment, chronic conditions going unnoticed, or even preventable emergencies. Unlocking this knowledge today could define the arc of your family’s health for decades to come.

Building Healthcare Fluency: Why Three Decades of Service Change the Game for Primary Care in Uganda
To be truly “fluent in healthcare” requires more than surface knowledge; it means having real, practical access to a medical ecosystem that supports you through preventive, acute, and chronic conditions. Primary care in Uganda has undergone a significant journey, evolving from basic outpatient visits to sophisticated, multi-disciplinary clinics capable of treating children, adults, and the elderly with a full suite of services. Whether managing maternal health, dental needs, or emergency crises, this fluency involves not just the presence of experienced doctors and nurses, but also systems for timely appointments, specialist access, and integrated insurance cover. Case Clinic and Case Hospital Medcare Insurance Services illustrate this paradigm, offering Ugandans the ability to confidently face health uncertainties with reliability.
The stakes are high for those who don’t navigate this space well. Lack of comprehensive knowledge about acute and ongoing care solutions can leave families exposed—leading to missed opportunities for early intervention or the stress of navigating emergencies without a network of prepared professionals. A cornerstone of effective healthcare is the ability to seamlessly transition from routine visits to specialist care or even urgent medical attention when seconds count. In Uganda, where health threats are varied and resources can sometimes be stretched, having a provider with a thirty-year track record means they’ve learned, adapted, and refined their methods to address real, everyday challenges. The result is a healthcare fluency that supports not only treatment, but also the prevention and ongoing management that keeps communities healthy and thriving.

How Primary Care with Case Clinic and Case Medcare Insurance Services Elevates Lives: Reliability, Access, and Peace of Mind
For three decades, Case Clinic and their Medcare Insurance Services have contributed to Uganda’s health sector as a seasoned guide, ensuring accessible, holistic care for every stage of life. As an expert contributor with over 25 years of holistic and quality service, they have honed an approach that spans the full spectrum of patient needs—offering everything from routine check-ups and preventive screenings to specialized care in cardiology, emergency medicine, and maternal health. Their experienced teams of physicians and support staff are distinguished by a collaborative ethos, ensuring patients receive care that is not only effective but also rooted in dignity and respect.
This continuity and knowledge translate into tangible benefits for those seeking reliable primary care in Uganda. By combining traditional in-person visits with telemedicine audio consultations, patients enjoy both convenience and breadth—enabling easy access regardless of circumstance. Moreover, their 24/7 emergency and critical care provision means urgent health issues are never left unattended, with skilled professionals ready to intervene in real-time. For families with children, adults managing chronic conditions, and elderly patients who need ongoing support, the assurance of skilled attention day and night offers a unique peace of mind not easily found elsewhere. Add to this their integration with accepted insurance plans, and the barriers to receiving expert care are significantly lowered.

The outcome is a setting that empowers people to live healthier, more confident lives—knowing that wherever they are on their health journey, a dependable system is in place to guide them. In a place as dynamic as Uganda, this strong safety net is more than a luxury: it’s a foundation for long-term wellbeing.
From Routine to Emergency: A Comprehensive Approach That Unites Preventive Care and Crisis Response
One of the enduring strengths of a truly fluent healthcare provider is the ability to seamlessly bridge everyday needs with high-stakes emergencies—whether it’s a routine health check, a paediatric concern, or a critical accident. Case Clinic’s model stands out precisely because the journey does not end at the first point of contact. Their structure is designed for holistic coverage, connecting primary care, specialist services, and a dedicated emergency department under a unified umbrella. This means a patient presenting with a minor health issue is in the same network as one experiencing severe trauma—supported by in-house specialists who work together, offering smooth transitions and follow-up from diagnosis to recovery.
With 24/7 emergency response, including open operating theatres, high-dependency units (HDU), and intensive care units (ICU), the continuum of care is more than just a promise. Highly trained staff and advanced medical facilities ensure no critical minute is lost when urgent needs arise. At the same time, ongoing availability for appointments, flexible scheduling, and preventive screening contribute to a system where health is managed proactively—catching problems early and engaging families in preventative action. It’s a model that has made a profound impact in Kampala over almost thirty years, blending rapid response with ongoing doctor-patient relationships that are key to healthier living.

Telemedicine and Flexibility: Meeting Uganda’s Modern Healthcare Challenges
Healthcare delivery today must adapt to the realities of a fast-paced, and sometimes unpredictable, environment. Case Clinic’s commitment to flexibility shines through their telemedicine/telehealth services—a confidential, secure way to consult with experienced professionals without always needing a physical visit. For many Ugandans, this removes crucial barriers: work obligations, family responsibilities, urban-rural divides, and even safety concerns. Audio consultations allow patients to seek medical advice, obtain diagnoses, or initiate treatment for non-urgent issues right from their homes or workplaces, ensuring that timely care remains within reach.
Beyond convenience, this innovation empowers individuals to be proactive about their health, catching potential issues before they escalate. Flexible appointment booking and a broad spectrum of accepted insurance plans further amplify access, strengthening the hospital’s mission to serve as a partner in long-term wellness rather than only a crisis responder. This agile, patient-centric mindset is not only about keeping pace with technology, but about making real improvements in how everyday healthcare is experienced and delivered across the country.
Insurance: A Critical Piece for Long-Term Care and Affordability
For many families, medical costs are an ever-present concern—even deterring them from seeking timely care. This is why integrated insurance services, such as those provided by Case Medcare, play a critical role in the healthcare ecosystem. By accepting a wide range of insurance plans, the hospital helps patients bridge the gap between high-quality medicine and financial accessibility, reducing the risk of catastrophic out-of-pocket expenses. Insurance also streamlines care by simplifying pre-approvals, authorizations, and ongoing management, ensuring that health decisions are guided by clinical needs rather than financial pressure.
This partnership with insurance providers not only safeguards household budgets, but also creates peace of mind for those navigating chronic, acute, or preventive care. Families, children, and elderly patients alike benefit from knowing that their path to recovery and health maintenance is secure—enabling a more empowered relationship with their providers. In this way, genuine fluency in healthcare emerges not just from clinical excellence, but from a full alignment with the financial realities faced by ordinary Ugandans.
Case Medical Centre’s Philosophy: Three Decades of Holistic, Collaborative, and Patient-Centered Care
The guiding philosophy behind Case Medical Centre’s long-standing reputation is deeply rooted in holistic service, quality outcomes, and a collaborative spirit. The institution operates with the core belief that healthcare should encompass routine prevention, acute emergency services, and specialist interventions—all seamlessly connected through integrated teams. From pediatric care to complex neurosurgery, every discipline works together to support the overall well-being of patients, reflecting an enduring commitment to both technical excellence and compassionate care.
By focusing on flexible scheduling, continuous availability, and the adoption of modern telehealth solutions, Case Medical Centre demonstrates a patient-centered mindset that prioritizes accessibility without ever compromising on standards. Their approach is both adaptive and forward-looking; as healthcare needs change, the institution evolves—incorporating new technologies, expanding services, and strengthening partnerships with insurance providers. This willingness to innovate, grounded in a nearly 30-year legacy, positions them as a trusted authority on what it means to be truly “fluent in healthcare”—ensuring families in Uganda receive care that anticipates the future while honouring the trust built over decades.
Above all, their mission is to enable individuals and communities to thrive, by making high-quality healthcare not just a service, but a foundational pillar of daily life.
When Emergency Strikes: First-Hand Assurance of Expertise and Commitment
For many, true confidence in a healthcare provider comes when confronted with the unexpected—a sudden accident, a life-threatening injury, or the anxiety of a loved one in crisis. The real impact of three decades of experience becomes clear in these high-pressure moments, where speed, specialized knowledge, and steadfast care can mean the difference between despair and hope. Ahmed Satti, a patient’s family member, captures this experience vividly in his story:
Excellent medical care and attention. Came in for a family member who had an accident and severe head trauma and fractured skull. The in house neurosurgeon Dr Hussein and his team did a fantastic job. They also continued to take care of my cousin and monitor him while he was in the ICU. I would highly recommend Case especially for emergencies.
Stories like Ahmed’s are a testament to the life-changing difference made by preparation, teamwork, and a culture committed to excellence. Whether it’s the ongoing monitoring in ICU or skilled surgical intervention, the hospital’s expert handling reflects decades of focus, investment, and learning. For anyone seeking a healthcare partner, these lived experiences offer both reassurance and an invitation to take the step toward proactive, connected care.
Redefining Healthcare Access: Uganda’s Path Forward with Expertise, Innovation, and Trust
In an environment where health is among the most precious of resources, being fluent in healthcare isn’t merely a skill—it’s a crucial advantage. As Uganda continues to face new medical challenges, the ongoing presence of dedicated institutions shaped by time, trust, and adaptability sets a new benchmark for what’s possible. Through a unique blend of preventive services, specialist care, progressive telemedicine, and insurance solutions, Case Clinic and Case Hospital Medcare Insurance Services have established themselves as leaders—modeling the future of primary care that is reliable, accessible, and tailored to real community needs.
Their authority in the field draws on nearly three decades of evolving practice and commitment, providing families and individuals with the confidence to navigate their health journey from the everyday to the extraordinary. The value of this expertise continues to transform patient experiences, redefine expectations, and deliver long-term benefits for all who walk through their doors. When it comes to being truly fluent in healthcare, there is no substitute for experience—and institutions grounded in both tradition and innovation point the way forward for Uganda’s health sector.
Contact the Experts at Case Medical Centre
If you’d like to learn more about how being fluent in healthcare with Case Clinic and Case Medcare Insurance Services could benefit your care experience, contact the team at Case Medical Centre. 📍 Address: 69, 8HFG+R24, 71 Buganda Rd, Kampala, Central Uganda 📞 Phone: +256 800 211005 🌐 Website: https://casehospital.org/
Case Medical Centre Location and 24-Hour Availability
🕒 Hours of Operation:📅 Monday: Open 24 hours📅 Tuesday: Open 24 hours📅 Wednesday: Open 24 hours📅 Thursday: Open 24 hours📅 Friday: Open 24 hours📅 Saturday: Open 24 hours📅 Sunday: Open 24 hours
 Add Row
Add Row  Add
Add 



Write A Comment